Imagine a bustling hospital ward, filled with the constant hum of medical equipment and the gentle murmur of conversations. But in one room, the air crackles with tension. You feel it the moment you step inside – the clenched jaw, the narrowed eyes, the barely suppressed anger. This is the reality of working with patients who exhibit aggressive behavior. It’s a complex situation that requires a deep understanding of underlying causes and a carefully crafted plan for intervention. This article will guide you through a holistic nursing plan for addressing aggressive behavior, designed to keep both the patient and staff safe while promoting a path towards healing.
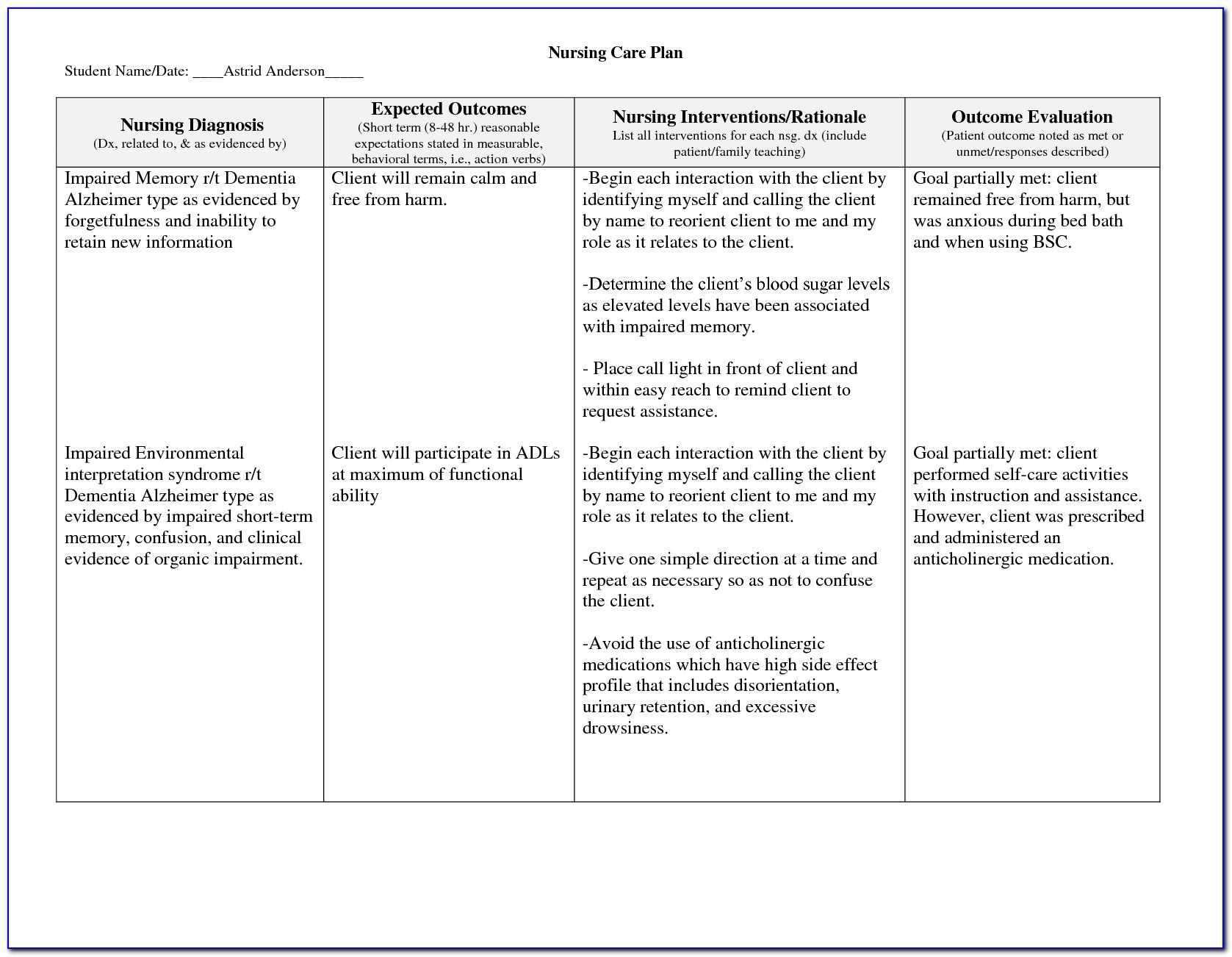
Image: templates.rjuuc.edu.np
Aggressive behavior isn’t inherently a personal attack. It’s a complex symptom of underlying distress. Stressors like physical pain, mental illness, substance withdrawal, or cognitive impairments can lead to heightened emotions and impulsivity. The goal of a nursing care plan is not to punish or restrain, but to understand the root of the behavior and provide the appropriate support. It’s about building trust, creating a safe environment, and providing the necessary interventions to help the patient regain control.
Understanding the Landscape: Unpacking Aggressive Behavior
Before we dive into the care plan, it’s vital to recognize that aggression exists on a spectrum. It can range from verbal threats and disruptive behaviors to physical violence. The first step in navigating this terrain is to understand the driving forces behind the behavior:
1. The Physical Component: Pain or discomfort can be a significant trigger for aggression. A patient with chronic pain, for instance, might lash out when they feel their physical needs aren’t being met.
2. Mental Health: Underlying mental health conditions, such as dementia, schizophrenia, or bipolar disorder, can also contribute to aggressive behavior. These conditions can lead to delusions, hallucinations, and difficulty managing emotions, making it challenging for the individual to control their impulses.
3. Substance Use: Withdrawal from drugs or alcohol can significantly increase agitation and aggression. The body is craving the substance it’s been deprived of, leading to a state of intense discomfort. This can manifest in erratic behavior and hostility.
4. Environmental Factors: Loud noises, interruptions, and unfamiliar surroundings can overstimulate already agitated individuals. It’s crucial to recognize that even seemingly insignificant factors can contribute to escalated behavior.
5. Personal History: Past trauma or abuse can lead to heightened responses to stress and anxiety. Individuals who have experienced severe trauma may react more intensely to situations that feel threatening or unsafe.
Building a Safe Haven: The Cornerstones of a Nursing Care Plan
A comprehensive care plan for managing aggressive behavior revolves around the following key pillars:
1. Assessment: Unlocking the Puzzle
- Gathering Information: Begin with a thorough assessment of the individual’s history, current medical conditions (including pain levels), medications, mental health status, and any recent stressors.
- Observation: Pay close attention to the patient’s behavior, including verbal cues, facial expressions, postures, and body language. Look for patterns or triggers that precede aggressive episodes.
- Collaboration: Involve the patient’s family, friends, or other healthcare providers to gain a well-rounded understanding of their baseline behavior and potential triggers.
Image: www.homage.sg
2. De-escalation Strategies: Navigating the Storm
- Calm and Assertive Communication: Use a calm and non-confrontational tone of voice, avoiding judgmental language or accusations. Speak clearly and directly, reframing any hostile statements into neutral observations.
- Active Listening: Show genuine interest in the patient’s feelings and concerns. Validate their experiences without agreeing with the aggressive behavior itself.
- Respectful Boundaries: Establish clear boundaries and set limits on behaviors that are inappropriate or unsafe. Be firm and consistent in enforcing these boundaries.
- Distraction and Redirection: When possible, use distraction techniques to shift the person’s focus away from the source of their frustration.
- Environmental Modifications: Reduce sensory overload by minimizing noise, clutter, and bright lights. Create a calm and peaceful environment conducive to de-escalation.
3. Safety First: Protecting Everyone Involved
- Immediate Intervention: If the situation escalates or becomes physically dangerous, prioritize safety by implementing emergency procedures. This may include removing other patients, calling for security, or using safety restraints as a last resort.
- Staff Safety Training: Ensure all staff are adequately trained in de-escalation techniques and safety protocols. Emphasize communication strategies and conflict resolution skills to defuse volatile situations.
- Environmental Design: Create a safe environment with enough space to move around comfortably, minimizing potential hazards like sharp objects or heavy furniture.
4. Understanding Medications: A Potential Ally
- Pharmacological Intervention: For patients with underlying mental health conditions, medications can play a vital role in managing aggression. Antidepressants, mood stabilizers, and antipsychotics can help stabilize mood, reduce impulsivity, and improve impulse control.
- Medication Management: Carefully monitor the patient’s response to medications and report any side effects or changes in behavior to the physician.
5. Building Bridges: Promoting Trust and Understanding
- Therapeutic Relationship: Develop a trusting relationship with the patient by demonstrating empathy, respect, and consistency. Show sincerity in your desire to help them, even when their behavior is challenging.
- Non-Judgmental Support: Reassure the patient that you are there to support them, regardless of their behavior. Avoid blaming, shaming, or making them feel invalidated.
- Positive Reinforcement: Identify and reward positive behaviors. For example, when the patient shows signs of calmness or self-control, acknowledge their efforts and offer verbal praise.
6. Empowerment and Control: A Path Towards Recovery
- Skill Building: Teach coping mechanisms and relaxation techniques to help patients manage stress and anger. This can include deep breathing exercises, mindfulness practices, or journaling.
- Cognitive Behavioral Therapy (CBT): Consider individual or group therapy to help patients identify their triggers, develop healthy coping strategies, and challenge negative thought patterns.
- Support Groups: Encourage patients to participate in support groups where they can connect with others who share similar experiences and receive peer support.
7. Documentation: A Record of Progress
- Thorough Records: Maintain clear and accurate records of all interactions, interventions, and outcomes. Include specific details about the patient’s behavior, triggers, and any changes in their condition.
- Communication: Share relevant information with other healthcare providers, family members, and support groups to ensure continuity of care.
Nursing Care Plan For Aggressive Behaviour
https://youtube.com/watch?v=uck9V0efZh4
Embracing the Journey
Navigating the complexities of aggressive behavior requires a compassionate and strategic approach. The nursing care plan, as outlined above, is a valuable tool to guide your efforts toward keeping the patient safe, fostering understanding, and working towards a path of healing. Remember, every patient is unique, and the best plan is one that’s tailored to their individual needs.
This journey may feel challenging, but it is a journey worth taking. By understanding the underlying factors, remaining patient, and utilizing effective communication, you can pave the way for a healthier and more peaceful future for both yourself and your patient.




