Imagine a patient lying in a hospital bed, their frail body struggling to recover from illness or surgery. They lack the energy to participate in their recovery and their skin appears pale and drawn. This is a scenario familiar to nurses, who often encounter patients struggling with imbalanced nutrition, a condition where the body isn’t receiving the necessary nutrients for optimal health and well-being. This article delves into the nursing care plan for imbalanced nutrition – less than body requirements, exploring the different aspects of managing this complex challenge.

Image: www.vrogue.co
Imbalanced nutrition – less than body requirements, also known as malnutrition, is a significant health issue affecting individuals across various age groups and disease states. It presents a serious threat to effective recovery and overall quality of life. This nursing care plan aims to equip nurses with the knowledge and tools needed to identify, assess, and address the needs of patients experiencing this nutritional deficit.
Understanding the Root Causes
The Complexities of Malnutrition
Malnutrition is often a symptom of an underlying medical condition, making it crucial to understand the root causes to effectively manage the patient’s care. Here are some common contributing factors:
- Disease Processes: Chronic illnesses such as cancer, heart failure, and chronic obstructive pulmonary disease (COPD) can impair appetite, absorption, and metabolism, leading to malnutrition.
- Social Determinants of Health: Poverty, food insecurity, lack of access to healthy foods, and social isolation can all contribute to malnutrition.
- Inadequate Intake: Conditions affecting the ability to eat, such as difficulty swallowing, impaired chewing, and decreased appetite, also play a role.
- Increased Nutrient Needs: During periods of illness, trauma, or surgery, the body’s nutrient requirements increase, making it more susceptible to malnutrition.
Recognizing the Signs
Recognizing the signs and symptoms of malnutrition is essential for early identification and timely intervention. Here are some key indicators that should raise concern:
- Weight Loss: Unintentional weight loss can be a significant indicator of malnutrition, especially if accompanied by other symptoms.
- Decreased Muscle Mass: Loss of muscle mass, particularly in the arms and legs, can be a sign of protein deficiency. This is often accompanied by weakness and fatigue.
- Fluid Retention: Edema, or fluid build-up in the tissues, can signal malnutrition due to a lack of protein and other essential nutrients.
- Dry, Brittle Skin: Lack of essential vitamins and minerals can contribute to dry, flaky skin, and impaired wound healing.
- Hair Loss: Hair loss or changes in hair texture can be a sign of protein deficiency or other nutrient deficiencies.
- Changes in Cognitive Function: Malnutrition can impair cognitive function, leading to impaired memory, concentration, and overall mental well-being.
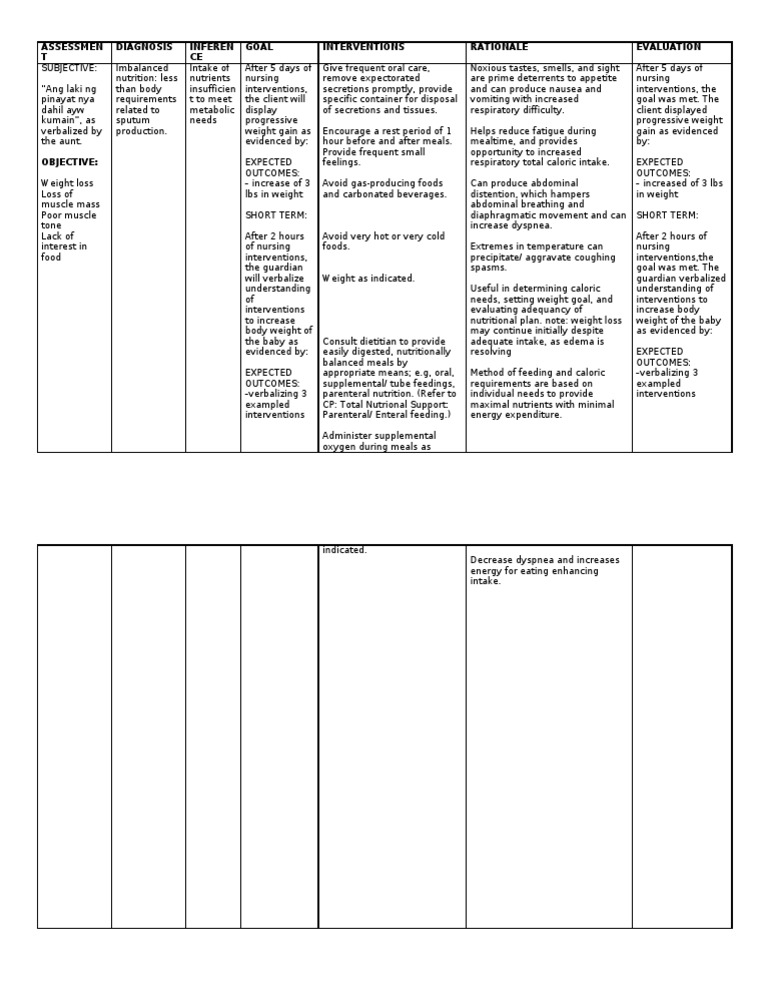
Image: www.vrogue.co
The Nursing Care Plan
1. Assessment and Monitoring
The nursing care plan for imbalanced nutrition begins with a thorough assessment to identify the specific cause of the malnutrition and the individual patient’s needs. This involves:
- Nutritional History: Gathering information about the patient’s dietary habits, food preferences, and any allergies or intolerances.
- Physical Assessment: Observing for signs and symptoms of malnutrition, including weight loss, muscle wasting, and skin changes.
- Laboratory Tests: Evaluating blood work, such as albumin and prealbumin levels, to assess nutritional status and identify deficiencies.
- Anthropometric Measurements: Measuring height, weight, body mass index (BMI), and mid-arm circumference to monitor nutritional status over time.
2. Nutritional Interventions
Based on the assessment, the nurse will develop a personalized nutritional care plan tailored to the patient’s needs. This may involve:
- Dietary Counseling: Providing education and guidance to patients on healthy eating habits, portion control, and food choices.
- Meal Planning: Working with registered dietitians to develop individualized meal plans that meet the patient’s specific nutritional needs and preferences.
- Oral Nutritional Supplements: Prescribing supplements to supplement dietary intake and provide additional calories, protein, and essential vitamins and minerals.
- Enteral Feeding: Providing nutrition through a tube inserted into the stomach or small intestine, also known as a feeding tube, for patients who cannot swallow or have impaired digestion.
- Parenteral Nutrition: Providing nutrition intravenously, typically for patients who cannot receive nutrition through their digestive system.
3. Enhancing Appetite and Oral Intake
Many factors can contribute to poor appetite in patients with malnutrition. The nurse can implement various strategies to stimulate appetite and enhance food intake:
- Small, Frequent Meals: Encouraging patients to eat smaller, more frequent meals throughout the day can reduce feelings of fullness and make meals more manageable.
- Pleasant Eating Environment: Creating a comfortable and relaxing atmosphere during meals can significantly improve appetite and enjoyment of food.
- Appealing Food Presentation: Making meals visually appealing by using attractive plating and garnishes can encourage patients to eat more.
- Food Preferences: Incorporating the patient’s favorite foods into their diet can help enhance their interest and willingness to eat.
- Nutritional Supplementation: Offering nutrient-rich snacks and beverages between meals can supplement dietary intake and provide additional calories and nutrients.
4. Collaboration and Support
Nurses play a vital role in coordinating care with other healthcare professionals to ensure the best possible outcomes for patients experiencing malnutrition. This includes:
- Registered Dietitians: Collaborating with registered dietitians to develop individualized nutrition plans and monitor patient progress.
- Physicians: Keeping physicians informed about the patient’s nutritional status and any changes or concerns regarding their diet.
- Social Workers: Working with social workers to address any socioeconomic factors contributing to malnutrition.
- Family Members: Involving family members in the care plan and educating them about proper nutrition and meal preparation can significantly impact patient outcomes.
5. Psychological Support and Education
The psychological impact of malnutrition can significantly affect patients’ recovery. Nurses can provide supportive interventions, such as:
- Listening to Concerns: Empathetically listening to patients’ concerns about their nutritional needs and offering support and encouragement.
- Education and Empowerment: Providing patients with education and information about healthy eating habits to empower them to make informed choices about their diet.
- Stress Management: Helping patients manage stress, as stress can affect appetite and worsen malnutrition.
Monitoring Progress and Evaluating Outcomes
Regularly monitoring the patient’s progress is essential to ensure the effectiveness of the nursing care plan. This involves:
- Monitoring Weight and Anthropometric Measurements: Tracking weight changes and other anthropometric measurements to assess the patient’s nutritional status and identify any improvement or deterioration.
- Assessing Dietary Intake: Assessing the patient’s actual food intake and comparing it to their prescribed meal plan to identify any areas for improvement.
- Evaluating Laboratory Test Results: Assessing changes in blood work, such as albumin and prealbumin levels, to monitor the patient’s nutritional response to the interventions.
- Assessing the Patient’s Subjective Experience: Ascertaining the patient’s subjective perception of their nutritional status and how they feel overall.
Based on the monitoring results, the nurse should adjust the care plan as needed to ensure it continues to meet the patient’s evolving needs. This may involve modifying the diet, adjusting the frequency of meals, or reevaluating the use of supplements.
Addressing Ethical Considerations
Ethical considerations play a crucial role in providing care to individuals with imbalanced nutrition. Nurses must respect patient autonomy and ensure that all nutritional interventions align with the patient’s values, beliefs, and preferences. This includes:
- Informed Consent: Obtaining informed consent from patients before implementing any nutritional intervention, ensuring they fully understand the risks, benefits, and alternatives.
- Respect for Patient Preferences: Respecting the patient’s preferences and choices, even if they differ from what the nurse considers optimal.
- Confidentiality: Maintaining confidentiality about the patient’s nutritional status and any discussions surrounding their care.
Future Directions
The field of nutritional care is continuously evolving, with ongoing research exploring new approaches to address malnutrition. Some promising areas include:
- Personalized Nutrition: Tailoring nutritional recommendations based on individual genetic profiles and microbiome composition to achieve optimal outcomes.
- Artificial Intelligence (AI): Utilizing AI algorithms to analyze nutritional data and predict nutritional needs for early intervention.
- Nutriceuticals: Exploring the use of targeted nutritional supplements to address specific nutrient deficiencies.
Nursing Care Plan For Imbalanced Nutrition Less Than Body Requirements
Conclusion
The nursing care plan for imbalanced nutrition – less than body requirements plays a vital role in optimizing patient care and maximizing recovery. By understanding the underlying causes, recognizing the signs, implementing effective interventions, and collaborating with other healthcare professionals, nurses can make a significant difference in improving the lives of patients who struggle with this challenging condition. Remember, the key to successful outcomes is a holistic approach that addresses not only nutritional needs but also the patient’s physical, emotional, and social well-being.




