Imagine a world where your senses are overwhelmed, bombarded by sights, sounds, and smells that feel chaotic and disorienting. This is the reality for many individuals experiencing disturbed sensory perception, a common yet often misunderstood condition. From the disorientation of a hospital stay to the sensory overload of autism, disturbed sensory perception can significantly impact an individual’s quality of life. This article delves into the intricacies of disturbed sensory perception and provides a comprehensive nursing care plan to help individuals navigate this challenging experience.
Image: nursestudy.net
Disturbed sensory perception, a term used in nursing, encompasses a range of sensory experiences that differ from the norm. It can involve alterations in any of the five senses – sight, hearing, touch, taste, and smell – leading to misinterpretations, misperceptions, or even hallucinations. For individuals experiencing altered sensory perception, the way they perceive the world around them can be distorted, impacting their ability to function, interact with others, and feel safe.
Understanding the Roots of Disturbed Sensory Perception
Disturbed sensory perception can stem from various underlying causes, making it crucial for healthcare professionals to understand its root to provide effective care. Some of the most common causes include:
- Neurological Conditions: Conditions affecting the brain, like strokes, traumatic brain injuries, dementia, and multiple sclerosis, can disrupt sensory processing, leading to distorted perceptions.
- Mental Health Conditions: Anxiety disorders, schizophrenia, and post-traumatic stress disorder (PTSD) can also contribute to sensory processing abnormalities, causing heightened sensitivity, misinterpretations, and even hallucinations.
- Medications: Certain medications, particularly those affecting the nervous system, can induce side effects that alter sensory perception.
- Substance Abuse: Alcohol and drug abuse can also impact sensory experience, leading to temporary or persistent perceptual changes.
- Sensory Overload: Even individuals without underlying conditions can experience sensory overload. For example, individuals with Autism Spectrum Disorder often have sensory sensitivities and may find certain sounds, textures, or lighting overwhelming.
The Importance of a Nursing Care Plan for Disturbed Sensory Perception
A nursing care plan is essential for individuals experiencing disturbed sensory perception as it provides structure, direction, and individualized interventions tailored to their unique needs. It serves as a roadmap for nurses, ensuring consistent, compassionate, and evidence-based care.
Key Components of a Nursing Care Plan
-
Assessment: The nursing care plan begins with a thorough assessment of the individual’s sensory perception, gathering information about their sensory experiences, any triggers, and their coping mechanisms. This includes questions about:
- What sensory experiences are particularly bothersome?
- What triggers their sensory issues?
- How do they manage these experiences?
- How does their sensory perception influence their daily life and interactions?
-
Diagnosis: Based on the assessment, the nurse will identify the nursing diagnoses related to the individual’s sensory perception, such as:
- Disturbed Sensory Perception: Visual (for vision-related issues)
- Disturbed Sensory Perception: Auditory (for hearing-related issues)
- Disturbed Sensory Perception: Tactile (for touch-related issues)
- Disturbed Sensory Perception: Gustatory (for taste-related issues)
- Disturbed Sensory Perception: Olfactory (for smell-related issues)
-
Planning: The nurse and the individual develop specific goals based on the diagnosis. These goals should be measurable, achievable, relevant, and time-bound (SMART). For example, goals might include:
- Reducing the frequency and intensity of sensory experiences.
- Developing coping strategies to manage sensory sensitivities.
- Improving communication and interaction with others.
- Creating a sensory-friendly environment to promote comfort and well-being.
-
Interventions: This section details the actions the nurse will take to help the individual achieve their goals. Interventions may include:
- Environmental modifications: Adjusting the environment to minimize sensory triggers, such as dimming the lights, reducing noise levels, or providing sensory-friendly tools.
- Sensory Modulation Techniques: A variety of strategies designed to calm the nervous system and regulate sensory input. These can include:
- Deep Breathing: Slow, deep breaths can help regulate the nervous system.
- Grounding Techniques: Focusing on the present moment by engaging the senses, such as describing the details of an object or the feel of a texture, can help reduce overwhelm.
- Sensory Integration: Utilizing sensory tools, such as weighted blankets, textured balls, or calming music, to provide sensory input can help regulate sensory responses.
- Communication strategies: Using clear, concise language, consistent routines, and visual aids can aid in effective communication for individuals with sensory processing difficulties.
- Education and Support: Providing education about sensory perception, coping mechanisms, and available resources can help the individual feel empowered and confident in managing their condition.
-
Evaluation: Regular assessments are essential to monitor progress and adjust the care plan as needed. This evaluation focuses on the individual’s progress toward achieving the set goals and identifying areas where further intervention might be necessary.
Expert Insights and Actionable Tips:
- Collaborate and Communicate: Healthcare professionals should engage the individual and their support system in the care planning process to ensure personalized care and informed decision-making.
- Sensory-Friendly Environments: Creating calm and predictable environments is critical in managing sensory perception. This involves minimizing sensory overload and providing sensory-friendly tools and resources.
- Personalized Care Plans: No two individuals experience sensory perception the same way. A tailored care plan, tailored to an individual’s specific triggers and coping strategies, is paramount.
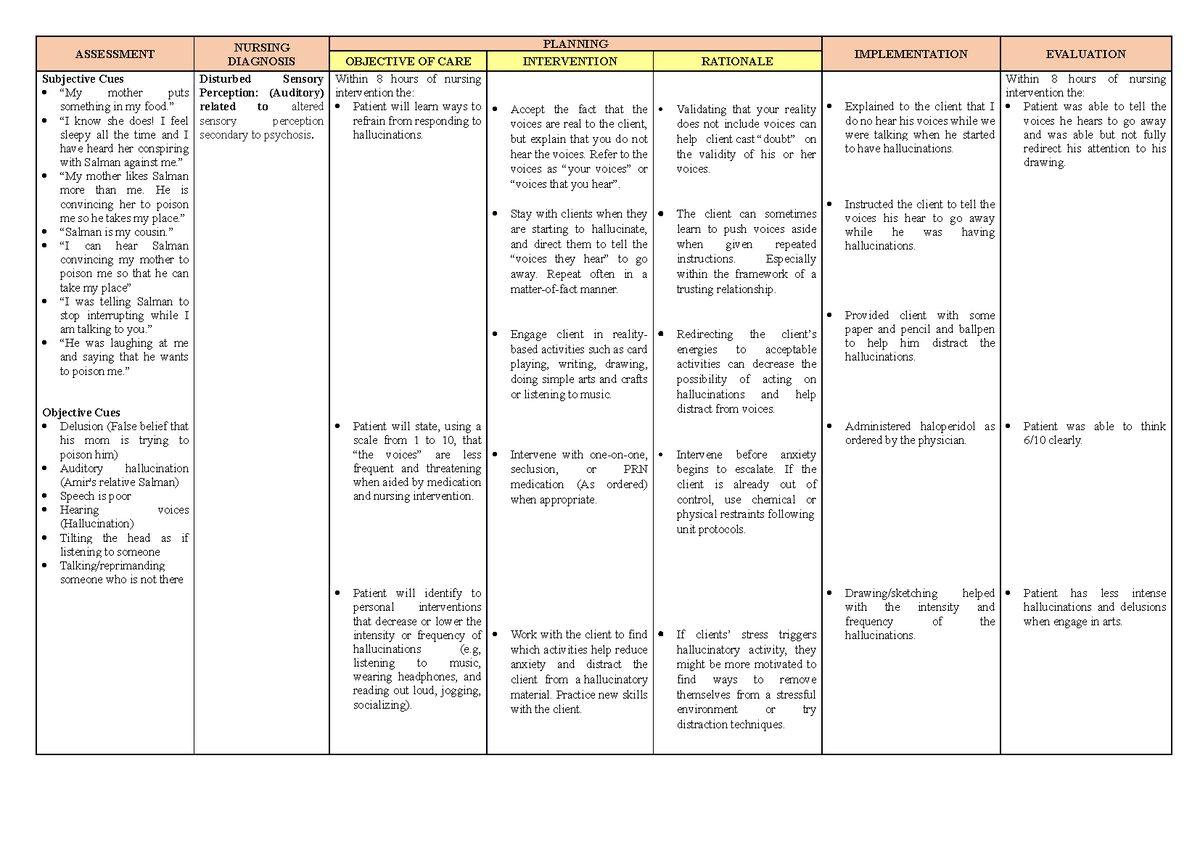
Image: www.vrogue.co
Disturbed Sensory Perception Nursing Care Plan
Conclusion
A disturbed sensory perception nursing care plan is essential for compassionate and effective care. By understanding the individual’s unique experiences, providing individualized interventions, and fostering a collaborative spirit, nurses can empower individuals to navigate the complexities of sensory perception and enhance their quality of life. Remember, sensory perception is a complex phenomenon, and with the right support, individuals can learn to manage their experiences and live fulfilling lives.




