Have you ever felt like the room was spinning, or as if you were floating on a boat in a rough sea? This disorienting sensation, known as vertigo, can be terrifying, leaving you feeling unsteady and unsure of your footing. But what happens when the world seems to be tilting, or when you feel lightheaded and faint? This is dizziness, a symptom that can be just as unsettling and disruptive to daily life. These two conditions, dizziness and vertigo, are commonly experienced by individuals across all ages, and understanding the underlying causes and appropriate nursing diagnoses is crucial for providing optimal care.
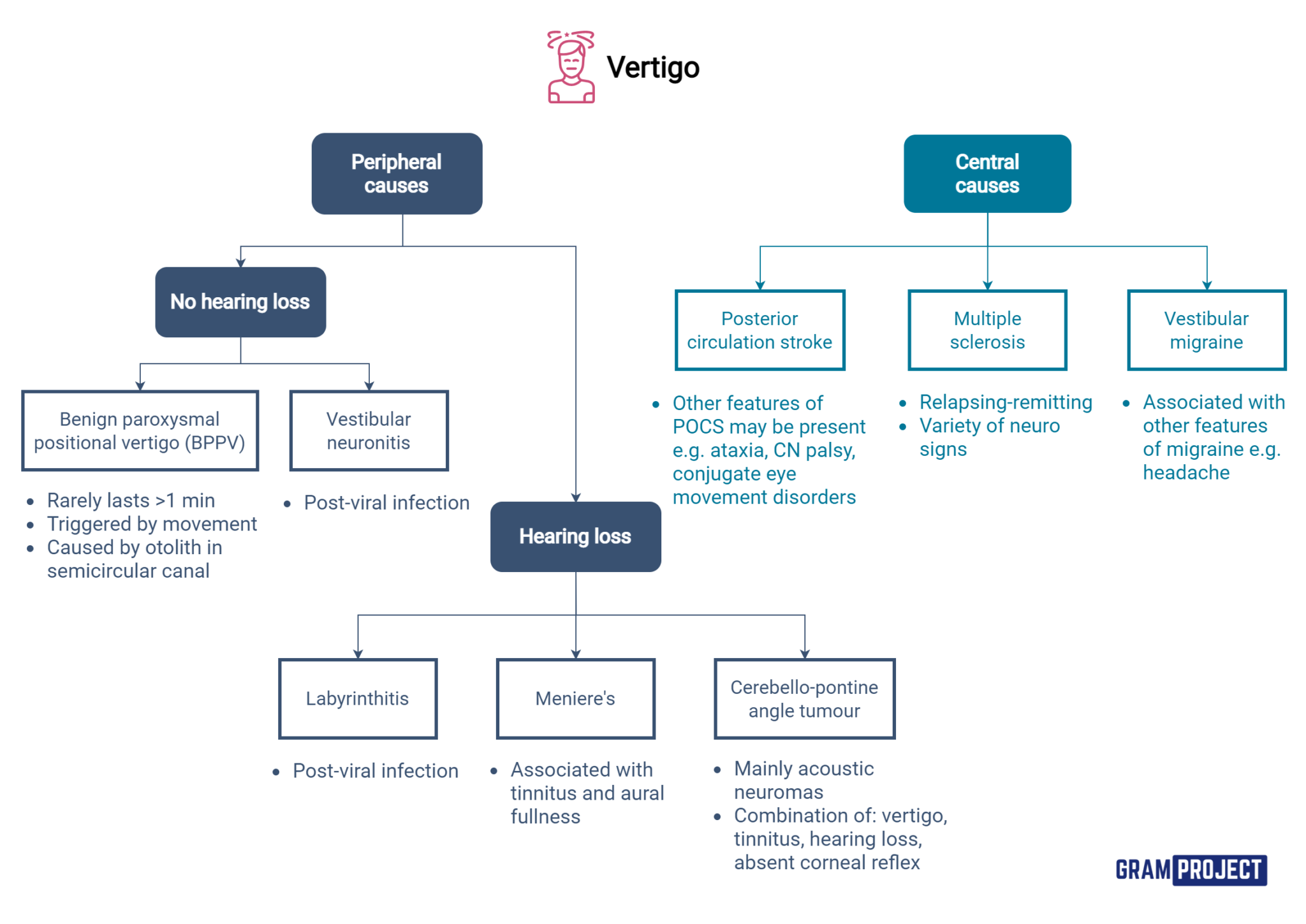
Image: gramproject.com
As nurses, we are at the forefront of patient care, tasked with deciphering the complexities of symptoms and developing personalized care plans. In this article, we will delve into the world of dizziness and vertigo, exploring the various nursing diagnoses that guide our interventions and promote patient recovery. We will discuss the diagnostic process, interpreting crucial assessment findings, and implementing evidence-based nursing interventions that aim to alleviate these debilitating symptoms and improve our patients’ overall well-being.
Understanding Dizziness and Vertigo: A Primer
Defining the Terms: Dizziness vs. Vertigo
Before diving into nursing diagnoses, let’s differentiate between dizziness and vertigo. While both involve a sensation of imbalance, they stem from distinct physiological mechanisms:
- Dizziness: A general term encompassing various feelings of lightheadedness, unsteadiness, faintness, or a sense of being off-balance. The feeling might be described as “room spinning” or simply a feeling of weakness. It often stems from issues related to blood flow, blood pressure fluctuations, or medications.
- Vertigo: A much more specific and often alarming condition, characterized by a sensation of spinning or whirling motion of either the self or the environment. This illusion of movement is often accompanied by nausea, vomiting, and difficulty maintaining balance. Vertigo primarily originates from problems within the inner ear, the central nervous system, or a combination of both.
The Labyrinthine Connection: Inner Ear and Vertigo
The inner ear plays a crucial role in maintaining balance and spatial orientation. It houses intricate structures, including the semicircular canals and the otoliths, which are responsible for detecting head movements and gravity. When these structures are affected—due to factors like infection, inflammation, or injury—it can disrupt the signals sent to the brain, leading to vertigo. This is why inner ear infections, known as labyrinthitis, can commonly trigger episodes of vertigo.

Image: mavink.com
Beyond the Ear: Exploring Other Causes
However, the culprit behind dizziness and vertigo is not always confined to the inner ear. A multitude of factors can contribute to these symptoms, often necessitating a comprehensive assessment to determine the underlying cause. Here’s a glimpse into some potential culprits:
- Cardiovascular Issues: Low blood pressure, heart arrhythmias, or even heart failure can trigger dizziness or lightheadedness due to inadequate blood supply to the brain.
- Neurological Conditions: A brain tumor, stroke, or even a migraine can affect balance and cause vertigo.
- Medications: Certain medications, including antidepressants, anti-anxiety drugs, and some antibiotics can lead to dizziness as a side effect.
- Metabolic Disorders: Diabetes or hypoglycemia can cause dizziness due to fluctuations in blood sugar levels.
- Dehydration: Lack of fluids can reduce blood volume, leading to lightheadedness.
- Anxiety and Stress: Psychological factors can also contribute to dizziness and vertigo, often manifesting as panic-related symptoms.
Nursing Diagnosis for Dizziness and Vertigo: Guiding Our Interventions
In the realm of nursing, accurate diagnoses provide a roadmap for effective care. To pinpoint the appropriate nursing diagnosis, a thorough assessment is paramount. The registered nurse plays a key role in this process, gathering information from the patient through a focused history, physical examination, and reviewing relevant medical records. Here are a few nursing diagnoses that may apply to patients experiencing dizziness and vertigo:
1. Risk for Injury
This diagnosis applies when the patient’s balance is compromised, increasing their risk of falls or other injuries. Factors that contribute to this risk include:
- Visual Disturbances: Vertigo can distort vision, making it difficult to navigate the environment safely.
- Impaired Mobility: The feeling of instability can hinder movement and make it difficult to walk independently.
- Cognitive Impairment: Conditions that affect cognitive function, such as dementia or certain medications, can add to the risk of falls.
2. Activity Intolerance
Patients experiencing dizziness often find it difficult to engage in even simple activities like walking, showering, or dressing, due to feelings of lightheadedness and fatigue. This can significantly impact their daily life and limit their participation in desired activities.
3. Risk for Falls
This diagnosis is particularly relevant for individuals at high risk of falling due to dizziness, and it emphasizes a proactive approach to prevent such events.
4. Impaired Physical Mobility
This applies when dizziness affects the patient’s ability to move around freely and independently. It highlights the need for interventions to promote mobility and regain functional independence.
5. Risk for Falls
This diagnosis is particularly relevant for individuals at high risk of falling due to dizziness, and it emphasizes a proactive approach to prevent such events.
Nursing Interventions: Tailored to Individual Needs
Once the nursing diagnosis is made, the next step is to develop a personalized care plan tailored to the patient’s specific needs and contributing factors. Interventions can vary widely, depending on the underlying cause and severity of the symptoms. Here’s a glimpse into some commonly employed interventions:
1. Promoting Safety
Safety is paramount when caring for patients experiencing dizziness. This involves:
- Home Safety Assessment: Identify potential hazards in the home environment, such as loose rugs, uneven floors, or slippery surfaces, and recommend modifications for a safer living space.
- Fall Prevention Strategies: Encourage the use of assistive devices like walkers or canes to maintain stability and reduce the risk of falls.
- Environmental Modifications: Ensure adequate lighting in the home, particularly in areas where the patient spends a lot of time.
- Supervision: Provide close supervision for patients who have difficulty maintaining balance and are at high risk for falls.
2. Managing Medications
Medication management plays a critical role in some cases, particularly if dizziness is a side effect of prescribed medications. This may involve:
- Reviewing Medications: Thoroughly review the patient’s medication list to identify potential contributors to their dizziness and explore alternative options if necessary.
- Dose Adjustments: Collaborating with the healthcare provider to adjust medication doses or discontinue problematic medications.
- Timing Adjustments: Adjusting the timing of medication administration to minimize side effects.
- Patient Education: Providing patients with comprehensive information about their medications, including potential side effects and how to manage them.
3. Addressing Anxiety and Stress
For patients whose dizziness is exacerbated by anxiety, addressing these underlying psychological factors is crucial. Here, we can implement:
- Relaxation Techniques: Teaching the patient relaxation techniques like deep breathing exercises, meditation, or progressive muscle relaxation to manage anxiety and stress.
- Cognitive Behavioral Therapy (CBT): CBT can help patients identify and challenge the negative thoughts and behaviors associated with their anxiety and dizziness.
- Support Groups: Connecting patients with support groups where they can share experiences and coping strategies.
4. Promoting Hydration
Ensuring adequate hydration is often essential, especially if dizziness is linked to dehydration. This involves:
- Fluid Intake: Encouraging patients to drink plenty of fluids throughout the day, particularly water, to maintain proper hydration.
- Electrolyte Balance: Monitoring electrolyte levels and addressing any imbalances that may contribute to dizziness.
5. Supporting Exercise and Physical Activity
While dizziness may make exercise seem daunting, gentle forms of exercise can actually help improve balance, strength, and overall health.
- Graduated Exercise Programs: Working with physical therapists to develop individualized exercise programs that gradually increase in intensity as the patient’s tolerance improves.
- Balance Exercises: Focus on balance exercises, such as standing on one leg or walking heel-to-toe, to improve proprioception and coordination.
- Strength Training: Including light strength training exercises to strengthen muscles that support balance and posture.
6. Relieving Nausea and Vomiting
Vertigo can often accompany nausea and vomiting. Here, we can offer:
- Antiemetic Medications: Administering antiemetic medications, as prescribed, to reduce nausea and vomiting.
- Dietary Modifications: Encourage bland foods like crackers or toast to settle the stomach and minimize further nausea.
- Hydration: Staying adequately hydrated is crucial when managing nausea and vomiting to prevent dehydration.
Looking Ahead: The Importance of Collaboration
Ultimately, managing dizziness and vertigo is a collaborative effort between the patient and the healthcare team. Nurses play a vital role by:
- Providing accurate and compassionate care: Empathizing with patients’ experiences and fostering a trusting relationship to encourage open communication about their symptoms.
- Implementing evidence-based interventions: Leveraging the latest research and best practices to guide interventions and maximize patient outcomes.
- Partnering with physicians: Closely collaborating with physicians to ensure the appropriate medical diagnosis and treatment plan.
- Educating patients: Empowering patients with knowledge and skills to manage their condition effectively.
Nursing Diagnosis For Dizziness And Vertigo
Conclusion: Navigating Labyrinthine Symptoms with Expertise
Dizziness and vertigo are conditions that can significantly impact a patient’s quality of life. Understanding the underlying causes and implementing appropriate nursing diagnoses empowers us to provide personalized care that alleviates symptoms, promotes safety, and helps patients regain their equilibrium. By diligently assessing, diagnosing, and intervening, we, as nurses, can navigate the labyrinth of dizziness and vertigo with expertise and compassion, empowering our patients to regain control over their lives and experience a greater sense of well-being.




