Imagine a patient recovering from a major surgery, their body fragile and vulnerable. The last thing they need is the added worry of potential bleeding. This is where the skill and expertise of nurses come into play. A key aspect of their role is implementing effective care plans to prevent and manage bleeding risks, promoting safe and successful recovery for patients.
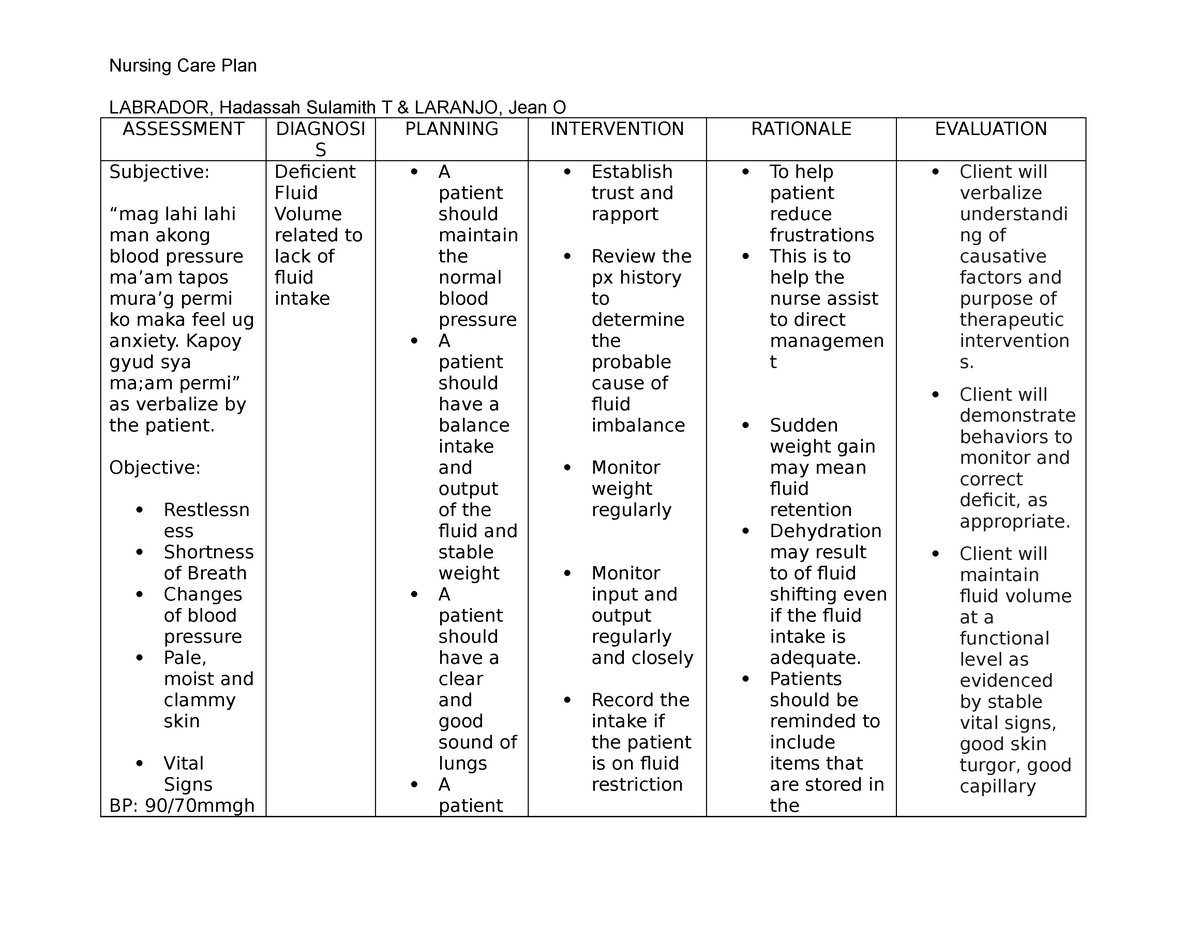
Image: www.hotzxgirl.com
This article delves into the multifaceted world of nursing care plans for patients at risk for bleeding. We’ll explore the reasons why these plans are crucial, the crucial assessments and interventions involved, and the importance of a collaborative approach to patient care.
Understanding the Risks: Unveiling the Causes of Bleeding
Before diving into the care plans, it’s crucial to understand the variety of factors that can put a patient at risk for bleeding. Here’s a breakdown:
Medications: A Double-Edged Sword
Many medications, while essential for treatment, can also increase the risk of bleeding. These include:
- Blood thinners (anticoagulants and antiplatelet medications): These medications prevent blood clots but also increase the risk of bleeding. Examples include aspirin, clopidogrel, warfarin, and heparin.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Commonly used to relieve pain and inflammation, NSAIDs like ibuprofen and naproxen can interfere with blood clotting.
- Corticosteroids: These powerful medications like prednisone, while helpful for many conditions, can weaken blood vessels and make them more prone to bleeding.
Medical Conditions: A Complex Landscape
Certain medical conditions also contribute significantly to the risk of bleeding. These include:
- Liver disease: The liver produces clotting factors essential for blood clotting. Liver disease can impair this function, leading to bleeding.
- Kidney disease: Kidney disease can affect blood clotting factors and make it harder for the body to stop bleeding.
- Hemophilia: A genetic disorder that affects the body’s ability to form blood clots, leading to prolonged and excessive bleeding.
- Cancer: Certain types of cancer, like leukemia, can impair blood clotting and increase the risk of bleeding.
Image: nurseslabs.com
Procedural & Surgical Risks: The Post-Procedure Challenge
Procedures and surgeries, especially those involving invasive techniques, increase the likelihood of bleeding. The risk of bleeding depends on the type of procedure, the patient’s overall health, and individual factors like bleeding disorders.
The Essential Toolkit: Nursing Assessments for Bleeding Risk
Nurses play a vital role in identifying patients at risk for bleeding. This involves a comprehensive assessment that includes:
Medications and Allergies: A Critical Review
A thorough review of the patient’s medications is paramount. This includes understanding all prescribed medications, over-the-counter drugs, and supplements. Nurses need to determine if any medications increase the risk of bleeding. Additionally, it’s essential to document any allergies that could impact treatment choices, such as allergies to medications used to control bleeding.
Medical History: Uncovering Past and Present Clues
A detailed medical history provides invaluable insights. Nurses need to gather information about past bleeding episodes, any existing medical conditions that contribute to bleeding risk, and family history of bleeding disorders. This information helps nurses understand the patient’s individual risk profile.
Physical Assessment: Observing Vital Signs and More
Physical assessment is crucial. This involves:
- Vital Signs: Monitoring vital signs like heart rate, blood pressure, and temperature helps detect early signs of bleeding.
- Skin Examination: Examining the skin for any signs of bruising, petechiae (tiny red or purple spots), or ecchymosis (larger areas of bruising) helps indicate bleeding under the skin.
- Gastrointestinal Assessment: Observing for signs of bleeding in the gastrointestinal tract, such as black or tarry stools, coffee-ground emesis, or blood in the vomit, is crucial.
- Neurological Assessment: This helps assess for signs of bleeding in the brain, such as altered mental status, headache, or seizures.
Laboratory Tests: Revealing the Blood’s Secrets
Blood tests play a crucial role in assessing the patient’s risk for bleeding. These tests help:
- Complete Blood Count (CBC): A CBC evaluates the number of red blood cells, white blood cells, and platelets in the blood. A low platelet count can increase the risk of bleeding.
- Prothrombin Time (PT) and International Normalized Ratio (INR): These tests measure how long it takes for blood to clot. Elevated PT and INR indicate a risk of bleeding.
- Partial Thromboplastin Time (PTT): This test evaluates the clotting ability of a specific part of the clotting process. An elevated PTT suggests a potential bleeding risk.
The Nursing Care Plan: Building a Safeguard
Once the assessment is complete, nurses develop a comprehensive care plan to prevent and manage bleeding risks. Here’s a breakdown of key elements:
Monitoring: Watching for Early Warning Signs
Constant monitoring is essential. Nurses meticulously observe patients for any signs of bleeding, including:
- Changes in vital signs: A dropping blood pressure, increased heart rate, or sudden change in respiratory rate can indicate internal bleeding.
- Changes in mental status: Confusion, lethargy, or decreased responsiveness could signify bleeding in the brain.
- Bleeding from the surgical site or other wounds: Nurses carefully inspect surgical incisions, dressing changes, and any other wounds for signs of bleeding.
- Abnormal drainage: Observing for blood-tinged drainage from body cavities, such as the chest or abdomen, is crucial.
- Gastrointestinal symptoms: Nurses monitor for changes in bowel habits, blood in the stool, or vomiting blood.
Medications: Managing Blood Clots Wisely
Medications play a central role in managing bleeding risks. Nurses administer medications as prescribed, including:
- Blood thinners: Carefully adjusted to maintain the correct therapeutic balance, preventing clots without increasing bleeding risk.
- Medications to control bleeding: These include medications like vitamin K, which helps with blood clotting, and antifibrinolytics, which help prevent the breakdown of clots (such as aminocaproic acid). The use of these medications is carefully considered depending on the cause of the bleeding and the patient’s condition.
- Pain medications: Nurses administer safe and effective analgesics (pain relievers) that do not interfere with blood clotting. This might include non-narcotic pain relievers or careful management of opioid doses.
Preventative Measures: Protecting the Vulnerable
Preventing bleeding is a key focus. Nurses implement strategies like:
- Pressure dressings: Applying direct pressure for a prolonged period aids in controlling bleeding. Nurses use sterile dressings and ensure proper pressure application.
- Sutures or staples: Surgical procedures often involve suturing or stapling to close wounds. Nurses ensure the proper application of sutures or staples to help minimize bleeding from wounds.
- Avoidance of invasive procedures: When possible, nurses and healthcare providers collaborate to avoid unnecessary invasive procedures to reduce the risk of bleeding.
- Careful handling of catheters and tubes: Nurses use gentle techniques when handling indwelling catheters and tubes to minimize the risk of bleeding from these sites.
- Fall prevention: Patients at risk for bleeding are more prone to falls, which can cause injuries and bleeding. Nurses implement fall prevention strategies, such as bed alarms, bedside assistance, and non-slip footwear.
Patient Education: Empowering Self-Care
Nurses play a critical role in educating patients and their families about bleeding risks and how to manage them at home. This includes:
- Understanding medications: Patients need to understand their medications, including dosages, potential side effects, and when to contact their healthcare provider. They should be instructed to avoid over-the-counter medications that can increase bleeding risks unless specifically authorized by their doctor.
- Recognizing signs of bleeding: Patients and families need to know the early warning signs of bleeding and when to seek immediate medical attention. Nurses provide clear, concise instructions on what to look for, such as unusual bruising, nosebleeds, vomiting blood, or bright red blood in the stool.
- Lifestyle modifications: Patients can make lifestyle changes to minimize bleeding risks. This includes avoiding activities that could cause trauma or injury, such as contact sports or heavy lifting. They should also be advised to use a soft-bristled toothbrush and electric razor to minimize risk of bleeding from gums or skin.
Collaboration: A Team Effort for Patient Safety
The care plan for patients at risk for bleeding is a joint effort. Nurses collaborate closely with:
- Physicians: Nurses work closely with physicians to adjust medication dosages, monitor patient progress, and make necessary changes to the care plan.
- Pharmacists: Nurses consult with pharmacists to ensure appropriate medication administration and to identify any potential drug interactions that may increase bleeding risks.
- Other healthcare professionals: Nurses collaborate with other healthcare professionals like physical therapists, occupational therapists, and social workers to provide comprehensive patient care and support.
- Patients and families: Nurses involve patients and families in decision-making and education, ensuring their needs and concerns are addressed.
Nursing Care Plan For Risk For Bleeding
Conclusion: Protecting Patients, Empowering Recovery
A comprehensive nursing care plan for patients at risk for bleeding is a crucial component of safe and effective patient care. By carefully assessing individual risks, monitoring for signs of bleeding, employing preventative measures, and educating patients and families, nurses contribute significantly to promoting patient safety and facilitating recovery. This collaborative approach underscores the vital role of nurses in providing individualized, compassionate, and evidence-based care for patients facing the challenges of potential bleeding.




